Recently, SMCPros featured the work of individuals and organizations in the community. We had an entry posted there, but we wanted to share it here as well.
Every day of the week, I find a call for help in my inbox. The people who write are unflinchingly honest about emotional breakdowns, job losses, and medical nightmares. They found a form on our website or our general email address, and sent something in the hopes that there is some help on the other end. Even though they have no idea they are writing to me, they are honest and candid to a degree that awes me. Because I forward these emails directly to our client advocates, Anna and Tom, almost none of them ever hear from me at all.
But nonetheless, they have come to the right place. In a system that still tends to treat people as less than, and with an illness that can make even the smallest obstacle too much to handle, they have run into a group of people who are dedicated to understanding their needs and helping them find their way. I work for a small non-profit, Mental Health Association of Minnesota. For over 70 years, we have helped people with mental illness be heard.
We don’t focus on what we think is important, we ask them what their goals are. For one client, it was making copies of correspondence without feeling like the hospital staff were looking over her shoulder. For Amanda, it was just sorting through the paperwork that meant the difference between a stable home and living on the street. For Kevin, it was trusting group home staff enough to tell them about his nutritional goals. It all matters because the person behind it matters.
Believing that we’re important and that we can take a concrete step towards recovery is absolutely necessary. Time becomes a real enemy when I feel depressed or anxious. I lose my sense of what things are like without that cloud hanging over me, much the same way that you might forget how good a full, deep breath feels after a long bout of the flu. Without hope and help, everything is too much, and every set back feels like the end of the world.
More than a decade ago, I was a patient at Abbot Northwestern, hospitalized a handful of times for suicidal behavior and thoughts. I was not responding well to medication, and every change in my prescription added another 15 or 20 pounds to my frame, until I could barely recognize myself in the mirror. In a matter of months, I had gone from zero involvement in the system to a head-first dive. It was frightening and lonely, full of people who didn’t believe me or listen to what I thought might help. I was on a unit with all kids, but many went days or even entire stays without seeing family.
I got daily visits from family. There were cards from my friends waiting for me when I got home. My internship supervisor came to the unit to make up for a lunch we were supposed to have. She even arranged a get-well call from her boss’s boss, a guy named Paul Wellstone. And from working in his office, I knew that it took phone calls all the way up the chain of command, and a scheduling effort. Far from taking away from the impact, it doubled it. You see, the point is that it’s not about one person who cares, it’s about entire families, communities, workplaces that do.
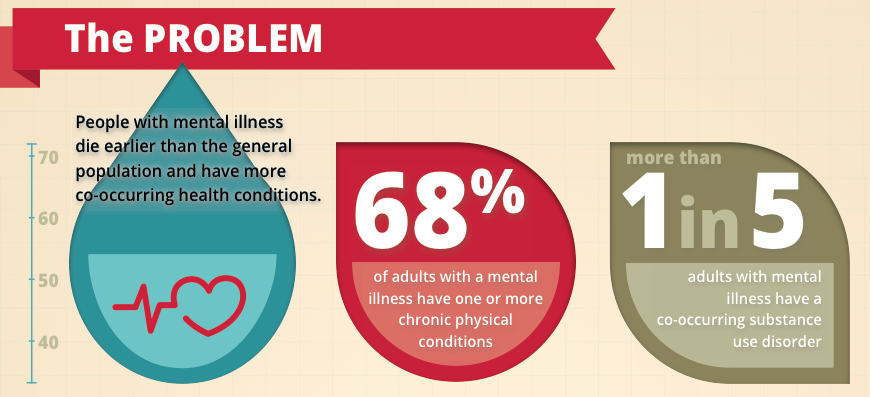
Mental illness is often chronic. It can be extremely painful and damaging. It is also true that people recover, leading wonderful and meaningful lives. They do so every day, but they almost never do it without support. MHAM takes phone calls and emails from anyone who is living in Minnesota or is concerned about a Minnesota resident who is having a hard time navigating the mental health system. We connect people with needed services, teach skills for self-advocacy and wellness, helping them live into their recovery.
I wanted to share this story with you so that you know two things. First. If you have a mental illness, and you don’t know where to turn, there is help. If it’s 2 AM when you’re reading this, and you’re in crisis, please call 800-273-TALK. It’s a different organization, but they are ready to connect with you, and believe me that it is worth it. But the next morning, I hope you email us at [email protected], or give us a call at 651-493-6634/800-862-1799.
Second. Whether or not you are living with a mental illness, do you agree with me that recovery shouldn’t be luck? There are plenty of ways for you to help. Drop us a line to find out more about volunteer opportunities, how to contact your legislators about life changing community mental health services, or our wellness education program. And yes, consider a donation. Our services may not be the easiest to fund in today’s economy, but that voice of hope is worth something. Personally, I think it’s worth quite a lot.
Ben Ashley-Wurtmann
Policy and Outreach Associate