When Sam first went to college, she had already been through a lot. She struggled with depression and anxiety throughout high school and had survived an abusive relationship. By the time her first semester of college started, she wanted to put it all behind her and start anew. What Sam did not know at the time, though, was that she was not only working against anxiety and depression, but also Post-Traumatic Stress Disorder (PTSD) that had not yet been diagnosed.
Without understanding what she was up against, Sam struggled over the next few years. She had blacked out memories that were resurfacing and was often afraid to go out with her friends. She numbed the pain by drinking and became addicted to painkillers. It was not until her senior year of college that Sam sought out help. She found a therapist whom she says helped change her life. “My therapist educated me on PTSD, helped me through the trauma through EMDR Therapy, helped me realized I wasn’t a failure and, most importantly, taught me to love myself.”
Sam spent five difficult years battling an illness she did not know she had. Unfortunately, her story is not unique. On average, the length of time between the onset of symptoms of mental illness and receiving treatment is ten years.
So how can we get young people the right help sooner? Mental Health Minnesota, a statewide organization that provides mental health advocacy, education and direct service, believes that an awareness and understanding of symptoms is an important first step.
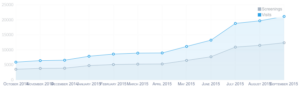
Mental Health Minnesota’s website hosts an anonymous online screening tool that aims to help people assess their mental health. There has been a tremendous increase in the online screening program, with more than 100,000 people taking the screening in the last year. That number is up from just around 7,000 in 2013. More than two-thirds of those screenings are being done by those between the ages of 18 and 24.
If young people are able to better understand what they may be dealing with sooner, they can seek out treatment earlier, and as a result, have a better quality of life. Sam strongly believes that had a screening been available to her earlier on, it would have been incredibly helpful to leading her to the correct diagnosis sooner.
Today, Sam is doing well: she is working on her recovery and has a passion for increasing awareness around mental illnesses. However, Sam’s story highlights the impact of the gap between onset of symptoms and treatment. When asked where she thinks she would be today if she hadn’t received the help she needed in five years instead of the average ten, she simply stated, “I don’t know if I would still be here.” However, she also wants to convey hope to others. “I have come to believe in the phrase ‘it gets better,’” said Sam. “I used to hate it when people said that to me, but now I realize why people say that. So, as much of a cliché as it is, things really do get better.”
Thursday, October 6, 2016, is National Depression Screening Day. If you are concerned about your mental health, you can take the anonymous screening at www.mentalhealthmn.org. The screening includes assessments for symptoms of depression, bipolar disorder, generalized anxiety disorder, posttraumatic stress disorder, adolescent depression, alcohol use disorder, substance use and eating disorders. At the end of the screening, you will see your results and access resources for help.
“We want people to know that recovery is possible, and that help is out there,” said Shannah Mulvihill, Mental Health Minnesota’s executive director. “A screening like ours is a first step—We want more success stories like Sam’s.”