
Kim, why did you decide to testify at the Legislature?
There was a bill before the House of Representatives that would have made changes to civil commitment, including requiring law enforcement to take some people living with mental illness into custody if they missed their weekly doctor appointments. As someone living with a mental health diagnosis, I knew that this type of heavy-handed approach to mental health care would not work, and that it would be in violation of people’s civil rights. I knew that the reason I was able to move into recovery from my illness was because I had mental health providers who saw me as a person of integrity and built trusting relationships with me. Knowing first hand how important it is to feel respected and supported by mental health providers, I felt that it was my duty as a citizen to speak out against this harmful bill.
What was it like to testify in front of your elected officials?
It was scary. I had five minutes to say what I wanted to say. I wrote my testimony out ahead of time and practiced it in front of the mirror. But it was challenging, because legislators are not always careful about how they talk about issues related to mental illness. The language some of them used was surprisingly antiquated and based on old stereotypes. I hadn’t prepared myself for that, so I felt a bit offended at times. But, I felt good about what I had to say because it came from my life experience. I also felt good because merely by being there and sharing my expertise, I was challenging those old stereotypes.
Aren’t there advocates out there who speak on behalf of people living with mental illness? Why didn’t you just let them do the work?
There are a lot of advocates at the Capitol trying to make sure that those of us who live with a mental health diagnosis get good care. They are usually family members, friends or providers of mental health care. I appreciate the work they do. They are the people who were there for me when I was sick. But, when it comes to truly understanding what it is like to live day to day with a mental illness, the people who are the true experts are the people who actually live with a mental illness. We are the people who know first hand what works and what doesn’t.
Therefore, I felt that in order to make a good case against the bill, someone needed to talk about what it is actually like to live with a mental illness. The unique perspective of someone living with mental illness is often missing in public conversation.
You say that the perspective of someone with lived experience is often missing? What do you mean by that?
When conversations about how mental health services are delivered in our state take place, people living with mental illness are rarely at the table. I think the reason for this is the perception that people with mental illness are not able to speak for themselves, or are too impaired to effectively be a part of those conversations. This perception is false. People living with mental illness are able to add an invaluable perspective to conversations. They are the experts.
I have found that since there are few opportunities for people like me who have lived experience to give input into important decisions, we need to sometimes invite ourselves to the table. That is why I signed up to testify against this bill that was being discussed by my elected officials.
I believe that it is important to point out that everyone living with a mental health diagnosis is unique, and that their experiences and perspectives are unique, too.
One voice of lived experience at the table is not enough. We need lots of people to be willing to speak up.
What are other ways people who live with mental illness can participate in public policy discussions?
- Anyone can call, email, or schedule a meeting with their representatives to voice their concerns! Find out who represents you here: https://www.gis.leg.mn/iMaps/districts/
- Almost every county in Minnesota has a local citizens mental health advisory council. Check with your county to see if there are openings, and apply to be appointed.
- The State of Minnesota also has a variety of citizen advisory councils related to mental health. You can check with the Minnesota Secretary of State’s office for a list of openings.
- Occasionally, the Department of Human Services or counties hold listening sessions to get feedback from citizens about issues related to mental illness. When those are announced, take the opportunity to participate and give your perspective.

 The theme this year addressed parity and equity for mental health. While great strides have been made in building Minnesota’s mental health system, there is still significant work to do to truly have parity and equity for mental health treatment and services.
The theme this year addressed parity and equity for mental health. While great strides have been made in building Minnesota’s mental health system, there is still significant work to do to truly have parity and equity for mental health treatment and services. “We were really happy to see so many people visiting their legislators this year in addition to attending the rally,” said Mulvihill. “It’s so important for our elected officials to hear directly from their constituents that mental health is important to them.”
“We were really happy to see so many people visiting their legislators this year in addition to attending the rally,” said Mulvihill. “It’s so important for our elected officials to hear directly from their constituents that mental health is important to them.” Mental Health Day on the Hill is just around the corner!
Mental Health Day on the Hill is just around the corner!
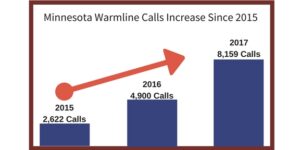 Calls to the
Calls to the  Jenna, can you tell us a little bit about yourself and what led you to start publicly sharing your recovery story?
Jenna, can you tell us a little bit about yourself and what led you to start publicly sharing your recovery story?