In any given year, 1 in 10 adults in the U.S. are affected by depression. Depression is a brain disorder that affects how you feel, think, and act. People with depressive illnesses do not all experience the same symptoms. The severity, frequency, and duration of symptoms vary depending on the individual and his or her particular illness.
Signs and symptoms include:
> Persistent sad, anxious, or “empty” feelings
> Feelings of hopelessness or pessimism
> Feelings of guilt, worthlessness, or helplessness
> Irritability, restlessness
> Loss of interest in activities or hobbies once pleasurable, including sex
> Fatigue and decreased energy
> Difficulty concentrating, remembering details, and making decisions
> Insomnia, early-morning wakefulness, or excessive sleeping
> Overeating, or appetite loss
> Aches or pains, headaches, cramps, or digestive problems that do not ease even with treatment.
> Thoughts of suicide, suicide attempts
There are different treatment options that can help, which may include medication, therapy, or combination of both. With effective treatment, the symptoms of depression will gradually get better.
If you are in crisis or thinking about harming yourself, or know someone who is, tell someone who can help immediately.
> Do not leave your friend or relative alone, and do not isolate yourself.
> Call 911 or go to a hospital emergency room to get immediate help, or ask a friend or family member to help you do these things.
> Call the toll-free, 24-hour hotline of the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255); TTY: 1-800-799-4TTY (4889) to talk to a trained counselor.
For more resources and information on depression and other mental health disorders, please visit:
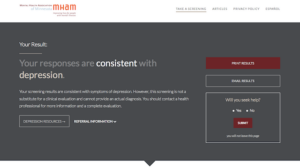
Online Mental Health Screening
The Mental Health Association of Minnesota has partnered with Screening for Mental Health, Inc. to provide free online screening for mood and anxiety disorders. This anonymous online assessment screens for depression, bipolar disorder, generalized anxiety disorder, and post-traumatic stress disorder. This screening is not a substitute for a diagnosis, but it will help determine whether or not a consultation from a health professional would be helpful. If you want to follow-up with a health provider, but have limited or no health insurance, MHAM can help find a sliding fee clinic or other medical coverage options. To speak with an advocate, call 651-493-6634 or 800-862-1799.
https://mentalhealthmn.org/be-informed/education-programs/online-screening-for-mood-and-anxiety-disorders
Get Help. Get Well.
Get Help Get Well helps people understand what to expect when seeking mental health care for the first time. Get Help Get Well includes information on…
> The first steps to obtaining care; healthcare providers to see initially; and factors to consider when seeking a healthcare provider.
> What may occur in the initial appointment; questions that may be asked by the health professional; and questions the patient may want to ask their health provider
https://mentalhealthmn.org/be-informed/get-help-get-well
Depression and Bipolar Support Alliance
The Depression and Bipolar Support Alliance (DBSA) is the leading peer-directed national organization focusing on the two most prevalent mental health conditions, depression and bipolar disorder. DBSA provides online resources and peer support groups.
http://www.dbsalliance.org/site/PageServer?pagename=home
Support Groups in Minnesota
You are not alone out there. Utilize support groups to share mental health needs and concerns affecting your life and the lives of others.
MHAM Sponsored Support Groups: DBSA Support Groups (Depression & Bipolar Support Alliance)
https://mentalhealthmn.org/mental-health-advocacy/individual-advocacy/access-to-health-care-and-community-services/support-groups/dbsa-support-groups
Other Minnesota Support Groups and Activity Centers
https://mentalhealthmn.org/find-support/resource-list/support-groups-activity-centers/all-support-groups
National Institute of Mental Health
The National Institute of Mental Health (NIMH) provides the latest research and information on depression and other mental health conditions.
http://www.nimh.nih.gov/health/topics/depression/index.shtml
MentalHealth.gov
MentalHealth.gov provides information and resources on mental illness for people experiencing a mental health disorder, family and friends, and other members of the community.
http://www.mentalhealth.gov/index.html